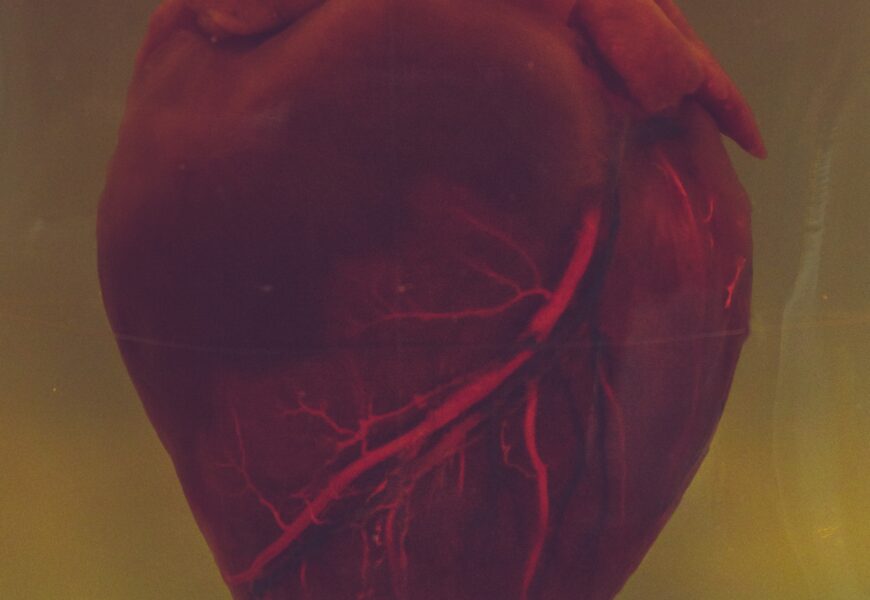
Photo Courtesy of Unsplash.
In the United States alone, one person dies every 36 seconds from cardiovascular disease. Globally, it is also the leading cause of death, claiming over 17 million lives each year. In cases of severe illness, heart transplants have shown great promise in increasing the life expectancy of patients with heart disease. About 75% of heart transplant recipients survive for 5 more years and about 56% survive for 10 more years. However, the average wait times for heart transplants are long, often exceeding 6 months, and some patients simply cannot afford to wait that long.
Therefore, scientists tend to refer to other modes of treatment which rely on managing chronic symptoms, such as hypertension (high blood pressure), diabetes mellitus, obesity, and high cholesterol. This approach, however, does not address the root cause of the problem, which is impaired heart functioning. Since heart cells do not have a mechanism to replace damaged tissue, scientists have become increasingly excited about the possibility of repairing or replacing damaged heart tissue using stem cells (unique cells that have the ability to divide for an extended period of time and differentiate into specialized cells, such as cardiac cells or nerve cells).
Regenerative medicine has been a topic of excitement among researchers for decades. In 1999, Anthony Atala, director of the Wake Forest Institute for Regenerative Medicine, was the first to implant lab-grown organs into several patients between 4 and 19 years old. In his method, he obtained bladder cells from the children and coaxed those cells into dividing on a scaffold (a structure that mimics the normal organ). The engineered bladders functioned normally and no ill effects were reported. “Pretty much I was able to live a normal life after,” said Luke, one of Atala’s patients.
More recently, Yoshiki Sawa, a professor of cardiovascular surgery at the University of Osaka’s medical school, and his team of Japanese researchers successfully transplanted lab-grown cardiac muscles into a human patient. The researchers first extracted adult stem cells from the patient’s blood or skin and genetically “reprogrammed” them into induced pluripotent stem (iPS) cells. They were then coaxed into 0.1-millimeter-thick sheets of cardiac tissue and grafted onto the diseased human hearts. According to Sawa, the cells do not seem to integrate into the heart tissue but rather release growth factors (proteins) that help regenerate blood vessels in the damaged muscle tissue and improve cardiac function. The team has conducted an operation on a patient in January 2020, marking the world’s first transplant of cardiac muscle cells.
The United States is also home to major breakthroughs in regenerative medicine. For decades, scientists have utilized embryonic stem cells to engineer heart muscle cells that are able to maintain synchronous breathing in a dish for hours. Despite this major feat, the creation of a working heart called for a more sophisticated technique. Doris Taylor, director of regenerative medicine research at the Texas Heart Institute (THI), has grown in her lab over 100 “ghost hearts” using protein scaffolds. She creates these scaffolds by first obtaining an animal heart and then “decellularizing” it by pumping a detergent through its blood vessels to “strip away lipids, DNA, soluble proteins, sugars and almost all the other cellular material from the heart, leaving only a pale mesh of collagen, laminins, and the extracellular matrix.” This heart does not necessarily have to be a human heart. She often finds pig hearts to be promising tissue because of their considerable safety and unlimited supply. She then “recellularizes” the heart by injecting it with millions of stem cells and attaching it to artificial lungs and a blood pump. Although her technique has only been used so far for growing animal hearts, she believes that it will eventually be used to create human heart transplants, thus, revolutionizing cardiovascular surgery and putting an end to organ shortage and anti-rejection drugs.
These groundbreaking results in regenerative medicine altogether have taken years of painstaking research to achieve. Taylor believes that her research is exceptionally close to building a working, human-sized heart, and Sawa says that his technique of grafting healthy cardiac muscle sheets onto the patient’s diseased heart tissue has already helped one of his patients move out of intensive care in just a few days. As the researchers gain more knowledge and get closer to the solution, however, they encounter more challenging obstacles. Sawa, for instance, has found that grafted cells do not always beat in synchrony. Researchers are also split on how these grafts work. On the other hand, investigating the best way to deliver cells still remains a challenge in Taylor’s research.
Stem cell research in tissue engineering could save millions of lives around the world; therefore, Taylor believes that “a coordinated approach among the researchers, clinicians, industry, regulatory bodies and, finally, society should be invigorated to catapult the field forward.” For instance, the “Twenty-first Century Cures Act” can help advance her work by facilitating cooperation among experts and regulatory bodies, providing for accelerated approvals for therapeutic tools in regenerative medicine, and improving the regulation of biologics products. She also maintains that tissue engineering efforts remain poorly funded and believes that more resources must be allocated before her studies can come to life. “There is a lot of dependence on societal benevolence,” she said. In an interview with RedMedNet, she also said that intense collaboration on a national and an international level is crucial and should be a priority, even though it could be challenging due to scheduling issues and differences in time zones.•